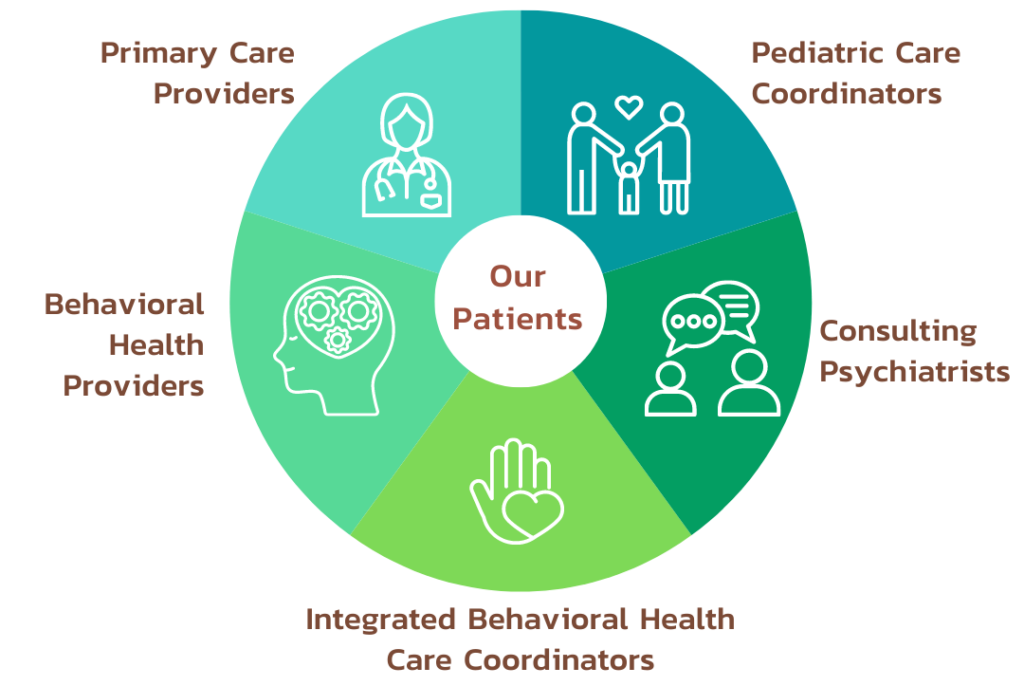
Typically, medical and behavioral health clinicians collaborate with each other and with patients and families to address health concerns identified during medical visits. Integrated behavioral health is found in primary care and in specialty settings, such as oncology, cardiology, neurology, pediatrics, and rehabilitation. Behavioral health clinicians often work right in the medical setting, or, if not onsite, are thoroughly integrated into the established procedures, team, and information systems.
Behavioral Health Integration
How would I recognize integrated behavioral health?
Behavioral Health Integration Program
Tran Urgent Care Wellness Centre support community primary care practices who want to integrate behavioral health clinicians (BHCs) within their practice. Our mission is to help you meet your patients’ behavioral health needs quicker and more effectively by integrating behavioral health services within the primary care practice.
Our Behavioral Health Integration (BHI) team will work with you to:
- Explore: Determine whether integration makes sense for your practice and what type of integration model is likely to work best for your patients, providers, system and community.
- Prepare: Help you hire, partner, train and prepare for integration.
- Implement: Support putting BHI into action.
- Maintain: Provide ongoing support to promote maintenance of the model and help your model reach its full potential.
Who can benefit from integrated behavioral health?
A growing body of research shows integrated behavioral health improves health and patient experience, while reducing unnecessary costs in time, money, and delays.
Integrated behavioral health offers many benefits:
What is Integrated Behavioral Health?
Behavioral health is an umbrella term that includes mental health and substance abuse conditions, life stressors and crises, stress-related physical symptoms, and health behaviors. Behavioral health conditions often affect medical illnesses.
Integrated behavioral health care blends care in one setting for medical conditions and related behavioral health factors that affect health and well-being. Integrated behavioral health care, a part of “whole-person care,” is a rapidly emerging shift in the practice of high-quality health care. It is a core function of the “advanced patient-centered medical home.”
Integrated behavioral health care is sometimes called “behavioral health integration,” “integrated care,” “collaborative care,” or “primary care behavioral health.” No matter what one calls it, the goal is the same: better care and health for the whole person.
Providers practicing integrated behavioral health care recognize that both medical and behavioral health factors are important parts of a person’s overall health. Medical and behavioral health clinicians work together as a team to address a patient’s concerns. Care is delivered by these integrated teams in the primary care setting unless patients request or require specialty services. The advantage is better coordination and communication, while working toward one set of overall health goals.
Why Integrate Behavioral Health Providers Within Primary Care?
- Improved Access: BHI results in significantly more youth receiving behavioral health care. After integration, clinics often see 2-3 times the number of their patients receiving behavioral health treatment.
- Improved Outcomes: Youth who receive integrated BH care are 66% more likely to have a better outcome than patients receiving usual care.
- Improved Patient Satisfaction: Families and youth prefer to receive behavioral health care within the primary care office.
- Improved Efficiency: BHI can reduce the amount of time primary care clinicians (PCCs) spend in the room, and may even improve reimbursement per minute.
- Improved Equity: BHI has been shown to reduce gaps in quality and access.

Patients with chronic health conditions are more likely to have related behavioral health concerns and often find it easier to improve chronic conditions when these concerns are also addressed.

Patients with chronic health conditions are more likely to have related behavioral health concerns and often find it easier to improve chronic conditions when these concerns are also addressed.

Medical providers appreciate having behavioral health partners available to help with problems the medical team doesn’t have enough time or training to address.

Providing integrated behavioral health care at the right times in the patient’s medical care can often offset the cost of providing the behavioral health care.